Abstract
Background: Patients with von Willebrand Disease (VWD) typically undergo a desmopressin acetate (DDAVP) responsiveness challenge at diagnosis to assess whether their coagulation deficits are sufficiently reversed following DDAVP administration. If responsive, patients can be treated with DDAVP in future when at increased risk of bleeding. Current practice assumes that DDAVP responsiveness remains constant over the adult lifetime, and therefore many adult patients are not re-tested. In the normal population, VWF plasma levels (VWF:Ag),VWF ristocetin activity (VWF:RCO) and coagulation factor VIII (FVIII:C) increase with age. This relationship has also been observed in patients with type 1 VWD. We hypothesized that DDAVP responsiveness also increased with age, and set out to investigate this relationship in patients with type 1 VWD.
Methods: We conducted a retrospective chart review of 106 patients enrolled at our center since 1990 who met diagnostic criteria for VWD and had undergone at least 1 DDAVP challenge. We recorded baseline, 1 hour, 2 hour and 4 hour post-DDAVP VWF related parameters for every patient when available. Baseline values were taken prior to DDAVP challenge, but may not reflect nadir levels required to diagnose VWD. We excluded patients on medications known to impact VWF and FVIII levels, and patients with types 2B, 2M and 3 VWD due to contraindication or lack of benefit with DDAVP. We stratified analyses by gender to control for the impact of estrogen on VWF and FVIII:C levels. Our primary outcome was DDAVP responsiveness in type 1 VWD, measured as changes in VWF:Ag, VWF:RCo, and FVIII:C levels one hour after DDAVP. As a secondary outcome, we determined these changes in type 2A VWD patients. Analyses were conducted using descriptive statistics, and Pearson and Spearman correlations were used to evaluate for the presence of linear and monotonic relationships, respectively.
Results: We had 90 patients (66 female) at our center with type 1 and 16 with type 2A (10 female) VWD who had undergone at least 1 DDAVP challenge. Blood type was available for 66 patients with type 1 VWD; 47 were type O (33 female) and 19 were non-type O (18 female). Mean age at DDAVP challenge for women with type 1 VWD was 23.2 years (SD 15.6) and 27.4 years (SD 19.8) for men. Mean DDAVP dose was approximately 0.3 mcg/kg, with no dose cap. Mean baseline VWF:RCo for type 1 VWD women was 0.39 IU/ml (SD 0.16) and 0.25 IU/ml (SD 0.14) for men, with concordant VWF:Ag mean levels. Mean baseline FVIII:C was 0.74 IU/ml (SD 0.33) and 0.49 IU/ml (SD 0.32) for the women and men, respectively. Blood type was available for 11 patients with type 2A VWD; 6 were type O (5 female) and 5 were non-type O (4 female). In the type 2A group, mean age at DDAVP challenge was 23.7 years (SD 19.0) in women and 50.7 years (SD 18.9) in men. Mean baseline VWF related parameters in type 2A VWD patients were, for women and men, respectively: VWF:Ag 0.48 IU/ml (SD 0.33), VWF:RCo 0.20 IU/ml (SD 0.09), FVIII:C 0.56 IU/ml (SD 0.14) and VWF:Ag 0.50 IU/ml (SD 0.30), VWF:RCo 0.18 IU/ml (SD 0.09), FVIII:C 0.57 IU/ml (SD 0.33).
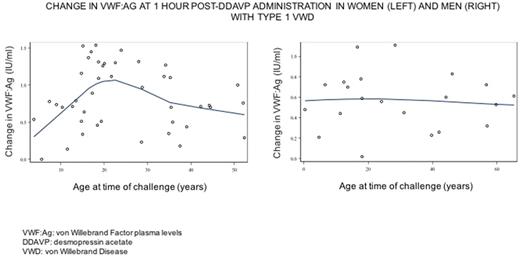
We excluded eleven type 1 VWD patients and one type 2A VWD patient due to medication use. The correlation between age and VWF-related responsiveness to DDAVP at 1 hour in women with type 1 VWD did not reveal a meaningful linear (VWF:Ag, Pearson -0.08, p = 0.62; FVIII:C Pearson 0.04, p=0.77) or monotonic (VWF:Ag, Spearman -0.03, p = 0.86; FVIII:C Spearman 0.12, p=0.40) relationship. However, when we explored the relationship graphically there was an indication of an age-related effect in women of child-bearing years for VWF:Ag, VWF:RCo and FVIII:C (see Figure 1). This finding was not observed in men with type 1 VWD, or in type 2A patients. Regression models including non-linear age terms may assist in explaining this trend.
Conclusion: In women with type 1 VWD, we found that responsiveness to DDAVP appears to be amplified around child-bearing years. This trend is reminiscent of the well-established relationship between serum estrogen levels and coaguability. To our knowledge, we have shown for the first time that post-pubertal women with type 1 VWD may have an enhanced ability to respond dynamically to DDAVP but only around this time period. We will confirm our findings with advanced statistical modeling. Future studies should assess whether these age-related changes of coagulation studies translate into meaningful lifecycle-related changes in the bleeding phenotype of type 1 VWD.
James: Bayer: Research Funding; Shire: Research Funding; CSL Behring: Research Funding. Sholzberg: Shire: Honoraria, Research Funding; CSL Behring: Honoraria, Research Funding; NovoNordisk: Honoraria; Octapharma: Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal